Epidemiological snapshot of dermatological conditions in a rural healthcare setting: a cross-sectional study in Belthangady, Dakshina Kannada District, Karnataka
1 Jul 2025
Epidemiological snapshot of dermatological conditions in a rural healthcare setting: a cross-sectional study in Belthangady, Dakshina Kannada District, Karnataka
Authors: Ankitha Adiga, Jacintha Martis, Ramesh Bhat M.
Dept of Dermatology, Father Muller Medical College, Karnataka, India
Abstract
Dermatological problems are a significant cause of morbidity in both rural and urban regions of low-resource countries, often accounting for a substantial proportion of visits to healthcare centres. Current knowledge about prevalence of dermatological disease largely stems from data from secondary and tertiary healthcare facilities, which may not accurately reflect disease patterns seen at the primary healthcare level.
This study aimed to explore the most common skin conditions and patterns of dermatology referral at Taluk Hospital in Belthangady, Dakshina Kannada District, Karnataka, India, as part of a district residency programme.
A cross-sectional study was conducted in the dermatology outpatient department over a 45-day period. All attending cases were included, and a thorough dermatological examination was performed. Cases requiring specialised tests or advanced treatment were referred to higher centres and excluded from the study.
A total of 227 patients were included, with an almost equal distribution of males (51.1%) to females (48.9%). The largest age group included patients between 11–20 years (24.2%), followed by those between 21–30 years (17.6%). Infective conditions were more prevalent (59.9%) than non-infective conditions (40.0%). Among communicable conditions, fungal infections were the most common (60.3%), particularly tinea corporis (62.1% of fungal cases). Eczema was the predominant non-communicable condition (46.2%), with hand eczema being the most frequent type (50% of eczema cases). Over-the-counter medication use prior to consultation was reported by 40.7% of patients. The follow-up rate was low, with only 24.7% of patients returning to the clinic.
This study highlights a high prevalence of communicable dermatological conditions in the Indian rural setting, with fungal infections being the most common. The findings underscore the importance of dermatology outreach clinics and the need for improved patient education on correct treatment and follow-up. Enhanced healthcare infrastructure and stricter regulations on inappropriate over-the-counter medications are crucial to improving dermatological care in rural regions.
Conflict of interest: None
Key words: Skin diseases; rural healthcare; district residency programme; healthcare access
Introduction
Dermatological problems are a significant cause of morbidity in low-resource countries, often accounting for a substantial proportion of visits to healthcare facilities. The distribution of skin diseases varies between countries1 and within different regions of the same country. In India, for example, the diversity in customs, religions, languages, climate, and socio-economic conditions across different regions leads to wide variation in dermatological patterns.2 Current knowledge about dermatological disease prevalence largely stems from data gathered at secondary and tertiary healthcare facilities, which may not accurately reflect disease prevalence seen at the primary healthcare level. Limited education often prevents patients from seeking treatment until skin symptoms become severe, and estimates suggest that up to 80% of affected individuals do not seek medical help at all.3
In rural areas, where primary care often represents the only accessible healthcare service, skin conditions are among the most frequently encountered health complaints.4 This cross-sectional study aimed to explore the most common skin conditions and patterns of dermatology referral in a rural setting. Forming part of a district residency programme by a dermatology junior resident, the study reports the pattern of skin diseases observed over 45 days in Taluk Hospital of Belthangady, Dakshina Kannada District, Karnataka.
Background
In 2022, the National Medical Commission launched the District Residency Programme (DRP) – a mandatory three-month training period for all postgraduate medical residents – with the aim of strengthening service provision within the district health system.5 The DRP was first implemented in April 2023, with residents assigned to various government healthcare facilities, ranging from district hospitals to subcentres and primary healthcare centres, to promote preventive and curative services at the rural healthcare level.6
Methods
All patients attending the dermatology outpatient department (OD) of Taluk Hospital of Belthangady, Dakshina Kannada District, Karnataka, within a 45-day period during February/March 2024 were included in the study. A brief, relevant clinical history was elicited, and a thorough dermatological examination was performed. Given the absence of investigative facilities, e.g., KOH mount and Tzanck smear, at the primary healthcare centre, skin diseases were diagnosed clinically based on their typical morphology. All skin conditions were categorised into two groups: communicable- and non-communicable disease. Patients needing specialised diagnostic tests or advanced treatment were referred to higher centres and were excluded from the study.


Results
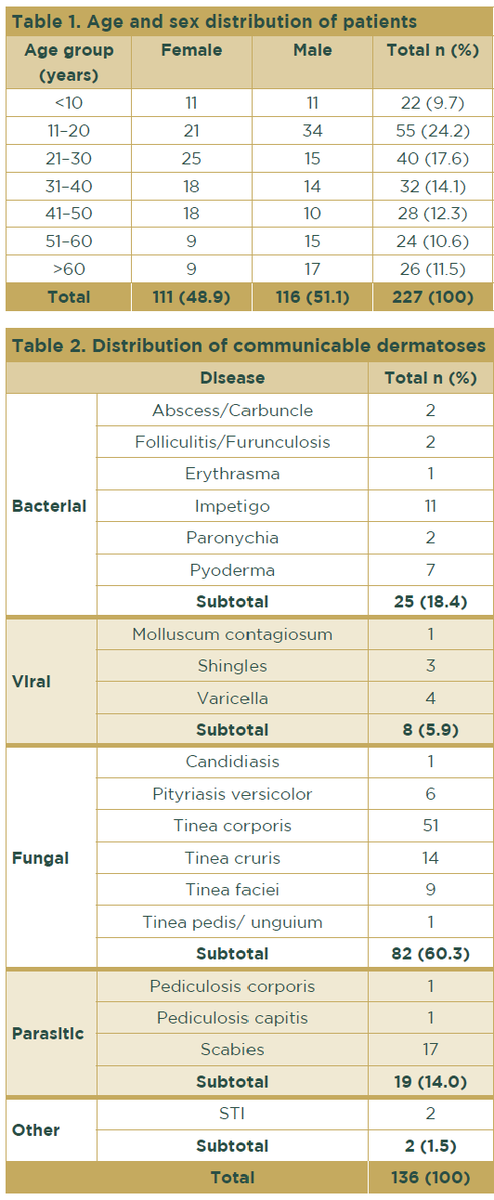
A total of 227 patients were included in the study. Of these, 116 patients (51.1%) were male; the largest age group (55 patients) represented individuals between 11–20 years (24.2%); the smallest age group comprised those below the age of 10 years (9.7%) (Table 1).
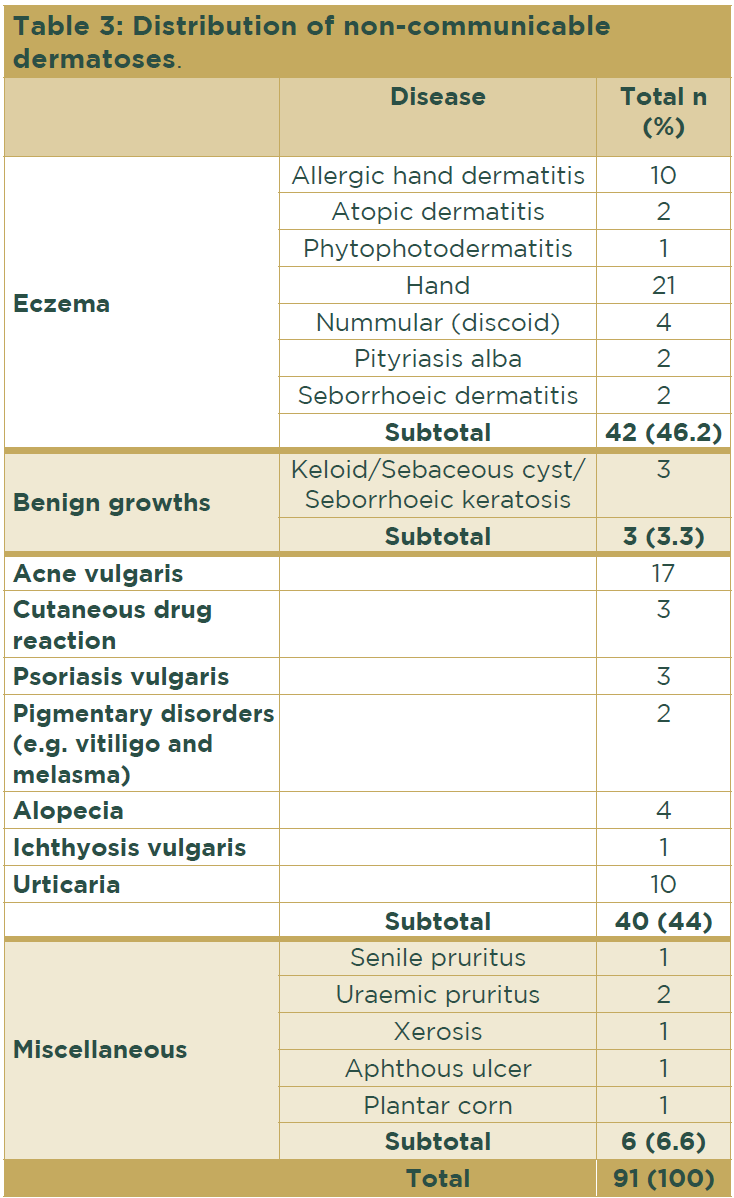
The prevalence of communicable disease (136 patients, 59.9%) surpassed that of non-communicable diseases (91 patients, 40.1%). Within the former group, fungal infections were the most prevalent, affecting 82 patients (60.3%), followed by bacterial infections, affecting 25 patients (18.4%) (Table 2). Among the fungal infections, the most frequent presentation was tinea corporis, identified in 51 individuals (62.2%). Scabies was the most common parasitic infestation, accounting for 17 patients (89.5%).
The prevalence of communicable disease (136 patients, 59.9%) surpassed that of non-communicable diseases (91 patients, 40.1%). Within the former group, fungal infections were the most prevalent, affecting 82 patients (60.3%), followed by bacterial infections, affecting 25 patients (18.4%) (Table 2). Among the fungal infections, the most frequent presentation was tinea corporis, identified in 51 individuals (62.2%). Scabies was the most common parasitic infestation, accounting for 17 patients (89.5%).

Two patients with tinea faciei are shown in Figures 1a and 1b; an example of impetigo is shown in Figure 2.
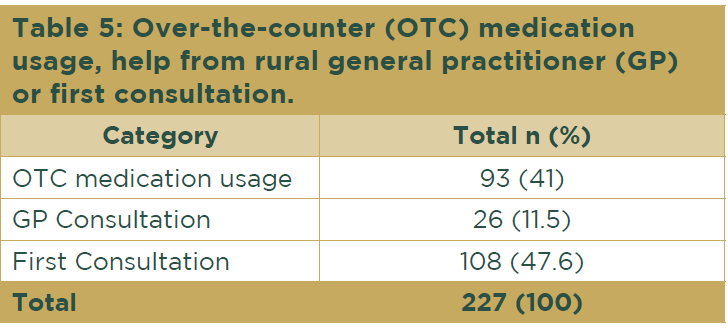
Overall, 93 individuals (41%) had used over-the-counter (OTC) medications obtained from pharmacies before seeking medical advice. In contrast, 26 patients (11.5%) had sought assistance from general practitioners, while 108 patients (47.6%) were attending their first consultation regarding their skin condition (Table 5).
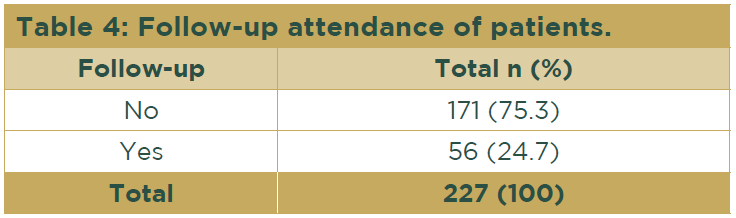
Among the non-communicable cases, eczema was the most common disorder, occurring in 42 patients (46.2%), followed by acne in 17 patients (18.7%). Within the eczema group, hand eczema was found in 21 patients (50%) (Table 3).
Of all the patients included in the study, only 56 (24.7%) returned for follow-up at the OD, while 171 patients (75.3%) were considered lost to follow-up (Table 4).
Overall, 93 individuals (41%) had used over-the-counter (OTC) medications obtained from pharmacies before seeking medical advice. In contrast, 26 patients (11.5%) had sought assistance from general practitioners, while 108 patients (47.6%) were attending their first consultation regarding their skin condition (Table 5).
Discussion
Results from this study reveal significant insights into the dermatological patterns found in this rural setting. The majority of dermatological consultations were for individuals aged 11–20 years, similar to findings from other studies that highlight a high prevalence of skin conditions among adolescents and young adults due to hormonal changes, lifestyle factors, and increased social interactions leading to higher exposure to infectious agents.1 Such observations highlight the crucial role of dermatology outreach clinics in managing paediatric skin conditions.
The predominance of communicable conditions over non-communicable conditions is consistent with other research findings from rural and semi-urban regions within low-resource countries. Fungal infections were the most common, with tinea corporis showing predominance (62.2% of fungal
cases). Similar findings were reported in studies from other parts of India and Southeast Asia, where dermatophytosis remains a significant public health issue due to hot and humid climatic conditions, poverty and household overcrowding, and lack of awareness about hygiene.7–9
Eczema was the most common non-infective condition, with hand eczema being particularly prevalent – a disease pattern that could be influenced by the occupational exposure common in rural areas, where manual labour is frequent. Acne, accounting for 18.7% of non-infective cases, predominantly affected the younger population, which is consistent with the age demographics of the study population. A lower percentage of people reported pigmentary disorders as a complaint, highlighting that cosmetic concerns are less prevalent among rural populations compared with those in urban India.
In rural areas, individuals often resort to using OTC medications without a proper diagnosis due to limited access to healthcare service provision and the ease of availability of OTC products. This practice can lead to inappropriate treatment and drug misuse, especially topical steroids, because many patients are unaware of potential side effects and correct usage. In this study, 41% of participants had used OTC drugs. Topical steroid abuse in rural areas is a significant public health issue that requires a multifaceted approach to its control, including education, stricter regulations, and improved access to healthcare. Addressing these challenges can help mitigate the adverse effects of OTC medications on skin and overall health, ensuring better health outcomes for rural populations.
The low follow-up rate (24.7%) seen in the study is concerning and reflects a broader issue of treatment adherence in rural settings; factors such as financial constraints, lack of awareness, and the perception of dermatological disease as ‘non-critical’ could contribute to this finding. Such factors can result in persistence or recurrence of disease, leading to secondary complications due to delay in seeking treatment or follow-up. This situation highlights the need for enhanced patient education and follow-up mechanisms to ensure better healthcare outcomes.
Conclusion
This study provides a snapshot of dermatological conditions in a rural healthcare setting, emphasising the prevalence of infective conditions and the challenges in treatment adherence. Addressing these factors through improved healthcare infrastructure and patient education could significantly enhance dermatological care in rural regions.
References
- Hay RJ, Johns NE, Williams HC et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol 2014; 134:1527–34.
- Hassan I, Anwar P, Bilquis S et al. Comparison of dermatoses seen in community health camps and a tertiary care centre in Kashmir. Indian J Dermatol Venereol Leprol 2014; 80:214–20.
- Grover S, Ranyal RK, Bedi MK. A cross section of skin diseases in rural Allahabad. Indian J Dermatol 2008; 53:179–81.
- Asbeck SM, Imo BU, Okobi OE, Dorcé-Medard J. The Dermatologic Care Needs of a Rural Community in South Florida. Int J Environ Res Public Health 2023; 20:3071.
- National Medical Commission: Post Graduate Medical Education Board (PGMEB). Implementation of District Residency Programme. Available at: https://www.nmc.org.in/MCIRest/open/getDocument?path=/Documents/Public/Portal/LatestNews/20221222070515.pdf (last accessed 10 March 2025).
- Desai SA, Ghatge R. District residency programme: An overview. J Family Med Prim Care 2024; 13:2177–8.
- Grills N, Grills C, Spelman T et al. Prevalence survey of dermatological conditions in mountainous North India. Int J Dermatol 2012; 51:579–87.
- Subramaniyan R. Pattern of Dermatoses Among Nicobarese in a Community Health Camp at Nancowry, Andaman and Nicobar Islands. Indian J Dermatol 2016; 61:187–9.
- Wootton CI, Bell S, Philavanh A et al. Assessing skin disease and associated health-related quality of life in a rural Lao community. BMC Dermatol 2018; 18:11.