French Guiana Tropical Dermatology Congress: a digest – Part I
8 Dec 2025
French Guiana Tropical Dermatology Congress: a digest – Part I
Authors:
Romain Blaizot [1], Quiterie Boscals de Réals [1], Geoffrey Grotta [1], Juliette Lebret [1], Pauline Oddo [1], Romain Chanlin [2], Clémentine Dehlin [2], Magalie Demar [2], Antoine Adenis [3], Kinan Drak [4]
- Department of Dermatology, French Guiana University Hospital, Cayenne, French Guiana.
- Parasitology-Mycology Laboratory, French Guiana University Hospital, Cayenne, French Guiana.
- Public Health Department, French Guiana University Hospital, Cayenne, French Guiana.
- Histopathology Department, French Guiana University Hospital, Cayenne, French Guiana.
Abstract
French Guiana is a French overseas territory in South America. It is mostly covered by deep rainforest and is inhabited by multiple populations, including Native Americans, Creoles, Maroons, and White Europeans. Due to its Amazonian location, its universal French healthcare system, and the presence of several ethnic origins and phototypes, French Guiana represents a unique setting in the field of Tropical Dermatology. The Dermatology Department of French Guiana University Hospital (formerly called Le Centre Hospitalier de Cayenne), in the capital city of Cayenne, has long experience in this specialism in the territory. In March 2025, the first French Guiana Tropical Dermatology Congress was held at the hospital, attracting participants from several countries. This article is Part I of a two-part series comprising a digest of several communications on tropical skin diseases of educational value from this congress. Part II will appear in a later issue.
Conflict of interest: None
Key words: French Guiana; tropical skin diseases; histoplasmosis; lobomycosis; chromoblastomycosis; tinea capitis.
Cutaneous histoplasmosis in French Guiana: a case series
Pauline Oddo, Antoine Adenis, Geoffrey Grotta, Magalie Demar, Romain Blaizot
Key learning points :
- Cutaneous histoplasmosis is endemic in South America, where it constitutes the most frequent opportunistic infection in people living with Human Immunodeficiency Virus (HIV).
- The infection is found in deeply immunosuppressed patients with less than 50 CD4/mm3.
- Cutaneous histoplasmosis can present with a wide range of mucosal or cutaneous lesions.
- Any suspect lesion in a patient with less than 50 CD4/mm3 in an endemic area should undergo a skin biopsy to look for Histoplasma capsulatum.
Introduction
Histoplasmosis, caused by Histoplasma capsulatum, is a fungal infection acquired through inhalation of airborne spores. In immunosuppressed patients – particularly those with very low CD4 counts (often < 100/mm3) and/or living with HIV – the infection can develop into a severe disseminated disease form. Histoplasmosis is endemic in French Guiana, where it constitutes the most frequent Acquired Immunodeficiency Syndrome (AIDS)-defining opportunistic infection.1
Often misdiagnosed as tuberculosis, histoplasmosis is now recognized as a neglected tropical disease, particularly in low-resource settings where deep tissue diagnostic facilities are limited. Cutaneous involvement, though less frequent than pulmonary disease, offers an accessible and cost-effective diagnostic clue. The incidence of histoplasmosis appears to be declining, probably due to earlier HIV intervention.2 However, cutaneous histoplasmosis may still be encountered by health workers caring for people living with HIV.
Methods
We present here a case series of cutaneous histoplasmosis seen in French Guiana between 2014 and 2024.
Results
All patients were young (less than 60 years of age) and had been living in French Guiana for at least 10 years. Five of the six patients were HIV-positive, with CD4 counts below 50. Histoplasmosis was the initial presentation in one patient, while the other five had already presented with opportunistic infections and had discontinued their HIV treatment for several years. The sixth patient was HIV-negative but had a concomitant human T-cell lymphotropic virus type 1 (HTLV-1) cutaneous lymphoma. All HIV patients presented with general health deterioration.
The extent of organ involvement varied: three patients had only cutaneous involvement, one had isolated mucosal lesions, one had both cutaneous and pulmonary disease, and one had cutaneous, lymph node, and bone marrow involvement.

Clinical manifestations were highly polymorphic. The case of isolated mucosal involvement presented with a granulomatous and ulcerated infiltration of the tongue (Figure 1). One patient presented with disseminated ‘prurigo-like’ papules, another with diffuse scaly macules resembling dermatophyte infection (Figure 2), and another with nonspecific, erythematous, scattered macules. One patient had coexisting Kaposi sarcomatous lesions that were infected with histoplasmosis, with violaceous vegetative papules on the palate and skin. The patient with HTLV-1–associated lymphoma had diffuse pseudotumoral lesions.

Skin biopsy was the initial positive diagnostic test in 5 out of 6 patients. Additional diagnostic yields included positive biopsy cultures (2/6), fungal blood cultures (2/4), urine cultures (1/2), and blood polymerase chain reaction (PCR) (1/1).
Due to the retrospective nature of the study, the duration of cutaneous clinical response to treatment could not be precisely determined. Overall, 4 of the 6 patients died, all of whom had concurrent opportunistic infections. Among the two surviving patients, one received itraconazole (400 mg twice daily for 4 weeks) followed by 6 months of non-adherence, and secondary prophylaxis with itraconazole for 2 years. The second surviving patient was treated with amphotericin B for 7 days, followed by itraconazole (600 mg for 48 hours and then 400 mg for 8 months), with treatment discontinued thereafter. This patient developed a pulmonary relapse two years later.
Discussion
Given the wide range of clinical presentations, consistent with previously reported literature, the diagnosis of cutaneous histoplasmosis remains challenging. These findings highlight the importance of considering histoplasmosis in any dermatological presentation in HIV-positive patients from endemic regions, especially when CD4 counts are below 50.
A comparison of lobomycosis and chromoblastomycosis in French Guiana
Geoffrey Grotta, Magalie Demar, Kinan Drak Alsibai, Romain Blaizot
Key learning points:
Lobomycosis
- Lobomycosis is a benign disease, although disseminated forms can be responsible for major functional and aesthetic impairment.
- Healthcare professionals in South America should be aware of its diagnosis, particularly in the case of keloid-like lesions.
- In French Guiana, lobomycosis displays a specific epidemiological pattern, largely affecting those involved with the gold mining industry.
Chromoblastomycosis
- Chromoblastomycosis is a chronic and neglected infection caused by dematiaceous fungi.
- Clinical presentation is characterised by slow and insidious progression, with verrucous, nodular, or ulcerative lesions that predominantly affect the lower limbs.
- In French Guiana, the first-line treatment is high-dose itraconazole, which can be accompanied by surgery in selected cases.
Introduction
Deep cutaneous mycoses are a neglected group of chronic fungal skin infections predominantly affecting individuals in tropical and subtropical regions. In French Guiana, lobomycosis and chromoblastomycosis represent two particularly underdiagnosed conditions, often encountered in populations with limited access to healthcare. These infections evolve slowly over years, leading to chronic lesions that are commonly mistaken for other dermatological disorders, resulting in delays in diagnosis and treatment.
Lobomycosis or Jorge Lobo’s disease, caused by Paracoccidioides lobogeorgii – previously known as Lacazia loboi – remains uncultivable and requires histological or mycological examination, typically through identification of chains of yeast-like cells in cutaneous biopsy.3 Surgical excision alone is rarely curative, with recurrence approaching 100%. Emerging evidence supports the use of multidrug therapy (MDT) with agents such as rifampicin, clofazimine, and dapsone, alongside surgical excision for better outcomes.4 Standard antifungal therapies are generally ineffective in lobomycosis, but new systemic treatments with posaconazole seem to be showing promising results in a few case series.5
In chromoblastomycosis, caused by pigmented fungi of the Cladophialophora and Fonsecaea genera, antifungal therapy with itraconazole or terbinafine should be combined with surgery and/or cryotherapy6,7 for patients who can afford these drugs. However, the cost of itraconazole remains an important barrier to treatment adherence.
Despite their similarities in chronic evolution and areas of endemicity, differences can be observed between these two mycoses.
Our objectives were to examine all cases of lobomycosis and chromoblastomycosis diagnosed in French Guiana since the creation of the Dermatology Department of French Guiana University Hospital (fomerly called Le Centre Hospitalier de Cayenne) in the 1950s until 2023 and to determine their epidemiological and therapeutic features.
Methods
All patients diagnosed with lobomycosis and chromoblastomycosis in French Guiana between 1955 and 2023 were included in this single-centre study.
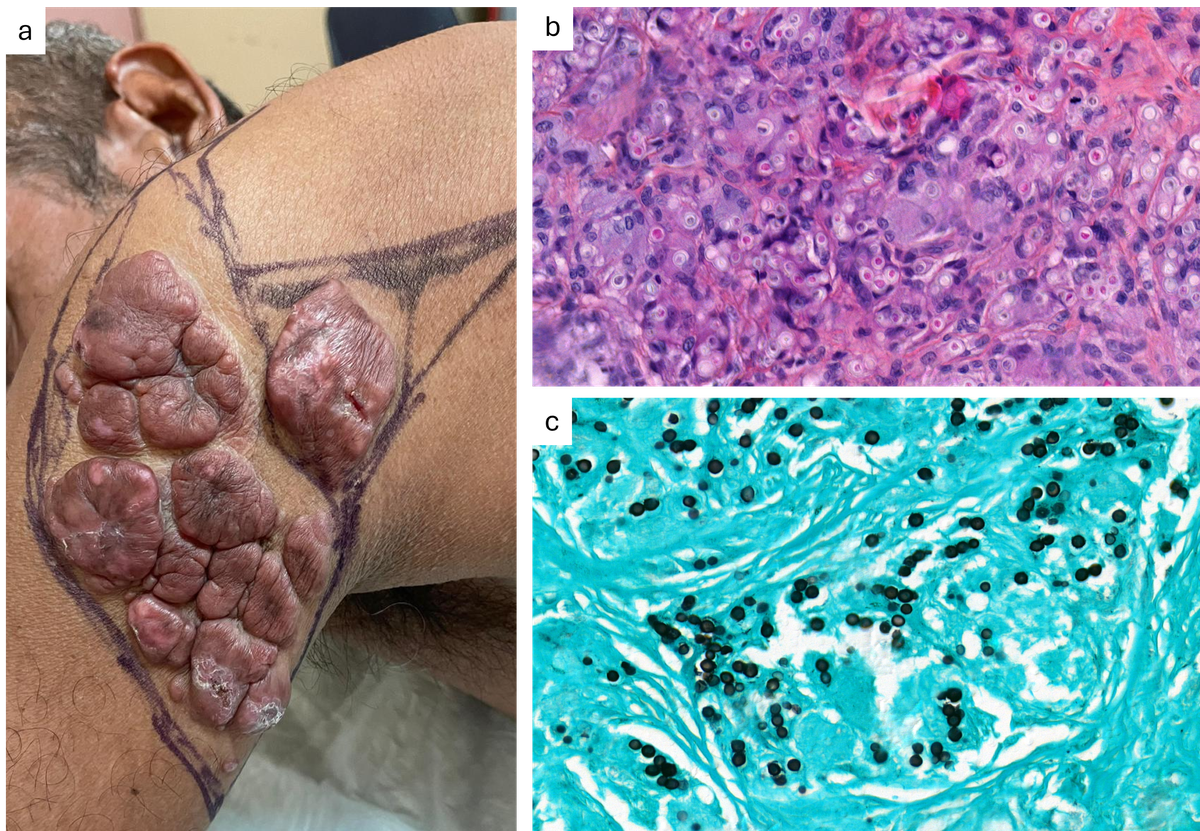
Results
In total, 31 cases of lobomycosis were recorded between 1959 and 2022. A notable epidemiological shift occurred after 2000, with 81% of cases emerging among Brazilian migrant gold miners (the affected population showed a marked male predominance of 84%). Clinical presentations included chronic, slow-progressing, keloid-like cutaneous lesions (Figure 3), found mostly on the lower limbs (55% of cases); multifocal involvement (several lesions involving at least two different body parts) occurred in 35% of cases. All patients with major disease forms (multifocal involvement or high fungal density) showed therapeutic failure or recurrence.
Meanwhile, chromoblastomycosis was observed in 23 patients between 1955 and 2023, primarily among local agricultural workers (48%). Twelve patients (52.2%) had a single lesion. The lower limbs were mainly involved (78.3%), followed by the upper limbs (21.7%). Clinical presentations included verrucous, cicatricial, or nodular lesions (Figure 4) in most cases, occasionally associated with pruritus or mild pain (26% and 17% of cases, respectively). Many therapeutic regimens have been used since the 1950s. Antifungal agents alone showed an efficacy rate of 33% compared with 66% when combined with surgery or cryotherapy.
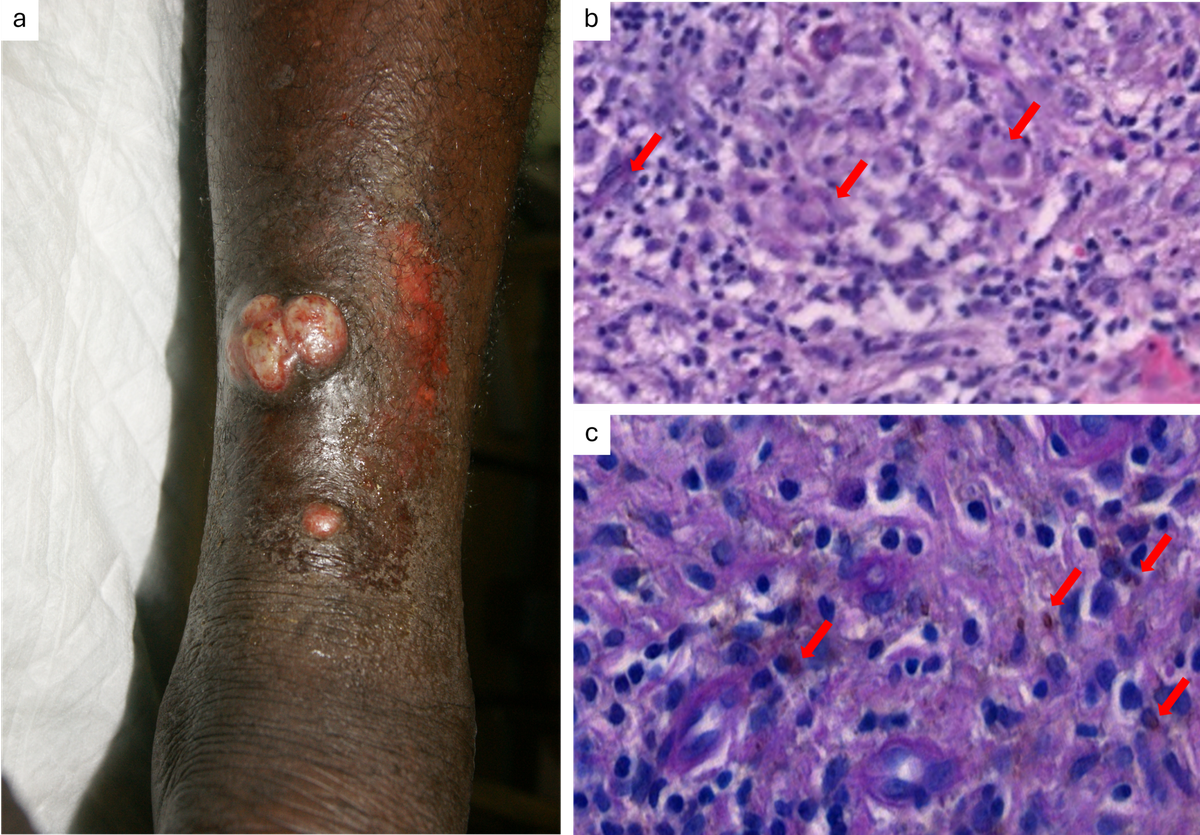
Discussion
Barriers to diagnosis and treatment in French Guiana include a lack of awareness, limited access to laboratory services in remote areas, patient mobility, and the absence of standardized treatment protocols. The mean duration before diagnosis was 4 years for both mycoses. Losses during follow-up were significant in both case series. Surgery remains the best therapeutic strategy for minor forms of disease.8 A combination of surgery and systemic antifungal therapy should be used for major or disseminated disease forms.
Experience of tinea capitis in French Guiana
Juliette Lebret, Geoffrey Grotta, Magalie Demar, Clémentine Dehlin, Romain Chanlin, Romain Blaizot
Key learning points:
- The first-line treatment for Trichophyton infection should be terbinafine, while itraconazole should be preferred for the treatment of Microsporum infection.
- Clinical presentation can be ill-suited for clinical diagnosis, given that up to 40% of Trichophyton cases can present with large patches usually associated with Microsporum infection.
- In French Guiana, as with the wider Caribbean, Trichophyton tonsurans is by far the most frequent pathogen responsible for tinea capitis.
Introduction
The epidemiology of tinea capitis is prone to variations over time and according to local ecology.9 French Guiana is an Amazonian overseas territory characterized by a high exposure to fungal and parasitic diseases. Although there is no published clinical data from this area, mycological data from 2009 suggest a specific epidemiology with most infections being caused by Trichophyton tonsurans.10 We sought to establish a clinical and biological description of tinea capitis epidemiology in French Guiana.
Methods
We collected all requests for mycological examination of scalp scales between 1 January 2017 and 31 December 2022 at the French Guiana University Hospital, the only referral centre for dermatology in French Guiana. Patients with a positive mycological examination were included in the study; identification was based on morphological criteria or Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry (MALDI TOF).
Results
A total of 322 requests for mycological examination of scalp scales were received. The test was positive in 150 cases (46.6%); patients were predominantly male (64.7%) and had an average age of 9 years. Most cases were caused by Trichophyton spp. (141/150, 94%); only 6% (9/150) arose from Microsporum spp.

Among the Trichophyton spp., the most common was T. tonsurans (102/141, 72.3%), followed by T. soudanense (22.7%), T. violaceum (2.8%), T. rubrum (1.4%), and T. interdigitale (0.7%). According to the available data, 79.2% (80/101) of these patients had multiple lesions; 70.8% (68/96) had alopecia; 59.4% (38/64) had small patches (Figure 5); 20.8% (21/101) had involvement of hairless skin; 9.2% (9/98) presented with clinical kerion.
Among Microsporum infections, the most frequent spp. was M. canis (6/9, 66.7%), followed by M. gypseum (2/9, 22.2%) and M. racemosum (1/9, 11.1%). Among these patients, multiple lesions were found in 71.4% (5/7) of cases; alopecia in 87.5% (7/8); large patches in 83.3% (5/6) (Figure 5); involvement of hairless skin, and kerion occurred in 37.5% (3/8) of patients.
Discussion
The epidemiology of tinea capitis in French Guiana is different from that observed in Europe, with a predominance of T. tonsurans infection being seen. While Microsporum infection represents 30% of cases in mainland France, the wider epidemiological landscape is changing, with a predominance of T. tonsurans now being seen in the United Kingdom11 and T. violaceum emerging in the rest of Europe.12 Current post-griseofulvin recommendations in mainland France include the use of terbinafine as an empirical treatment, although itraconazole should be preferred in Microsporum infection. In our study, the importance of parasitic identification was confirmed; more than 40% of Trichophyton cases presented with large plaques, suggesting an atypical presentation ill-suited to clinically-based diagnosis and treatment. Hair microscopy could help differentiate between pathogens, with an endothrix pattern (involvement of the hair shaft) in T. tonsurans and an ectothrix pattern (confined to the hair surface) with M. canis. The Wood lamp examination would be another means to distinguish M. canis (yellow-green fluorescence) from T. tonsurans (no fluorescence). This study presents the first data concerning tinea capitis in French Guiana, showing a ‘French American overseas’ epidemiology similar to previous studies in Martinique and Guadeloupe. This study also shows the persistence of severe presentations with kerion among French Guiana children.
References
- Morote S, Nacher M, Blaizot R et al. Comparison of disseminated histoplasmosis with and without cutaneo-mucous lesions in persons living with HIV in French Guiana. J Fungi 2020; 6:133.
- Morote S, Nacher M, Blaizot R et al. Temporal trends of cutaneo-mucous histoplasmosis in persons living with HIV in French Guiana: early diagnosis defuses South American strain dermotropism. PLoS Negl Trop Dis 2020; 14:e0008663.
- Vilela R, de Hoog S, Bensch K et al. A taxonomic review of the genus Paracoccidioides, with focus on the uncultivable species. PLoS Negl Trop Dis 2023; 17:e0011220.
- Gonçalves FG, Rosa PS, Belone A de FF et al. Lobomycosis epidemiology and management: the quest for a cure for the most neglected of neglected tropical diseases. J Fungi (Basel) 2022; 8:494.
- Bustamante B, Seas C, Salomon M, Bravo F. Lobomycosis successfully treated with posaconazole. Am J Trop Med Hyg 2013; 88:1207–8.
- Valentin J, Grotta G, Muller T et al. Chromoblastomycosis in French Guiana: epidemiology and practices, 1955-2023. J Fungi (Basel) 2024; 10:168.
- Ameen M. Chromoblastomycosis: clinical presentation and management. Clin Exp Dermatol 2009; 34:849–54.
- Grotta G, Couppie P, Demar M et al. Fungal density in lobomycosis in French Guiana: a proposal for a new clinico-histological and therapeutic classification. J Fungi (Basel) 2023; 9:1005.
- Gangneux J-P, Miossec C, Machouart M et al. Epidemiology and management of tinea capitis in France: A 6-year nationwide retrospective survey. Med Mycol 2024; 62:myae047.
- Simonnet C, Berger F, Gantier J-C. Epidemiology of superficial fungal diseases in French Guiana: a three-year retrospective analysis. Med Mycol 2011; 49:608–11.
- White JML, Higgins EM, Fuller LC. Screening for asymptomatic carriage of Trichophyton tonsurans in household contacts of patients with tinea capitis: results of 209 patients from South London. J Eur Acad Dermatol Venereol 2007; 21:1061–4.
- Fuller LC. Changing face of tinea capitis in Europe. Curr Opin Infect Dis 2009; 22:115–8.