The rise of sporotrichosis in Latin America: urgent need for a One Health response
8 Dec 2025
The rise of sporotrichosis in Latin America: urgent need for a One Health response
Authors:
Eduardo M. M. Falcão [1] [2], David J. Chandler [3] [4]
- Department of Dermatology, Instituto de Dermatologia Prof. Rubem David Azulay, Santa Casa da Misericórdia do Rio de Janeiro, Rio de Janeiro, Brazil.
- Department of Dermatology, Laboratório de Pesquisa Clínica em Dermatologia Infecciosa, Instituto Nacional de Infectologia Evandro Chagas, Fundação Oswaldo Cruz (Fiocruz), Rio de Janeiro, Brazil.
- Dermatology Department, Brighton General Hospital, University Hospitals Sussex NHS Foundation Trust, Brighton, UK.
- Department of Global Health and Infection, Brighton and Sussex Medical School, Brighton, UK.
Abstract
Sporotrichosis is a subcutaneous fungal infection that is increasingly recognized as a public health concern, particularly in Brazil, where disease caused by S. brasiliensis has become more frequent. The infection is mainly transmitted through environmental trauma or zoonotic transmission, notably from cats. Sporotrichosis is predominantly a cutaneous infection, with lymphocutaneous and fixed cutaneous forms being most common. Systemic involvement can occur, especially in immunosuppressed individuals. While itraconazole is the first treatment of choice, potassium iodide and terbinafine are alternatives for specific cases. Severe cases may require more intensive therapies such as liposomal amphotericin B or adjuvant surgical treatments. Sporotrichosis remains a significant public health concern, especially in hyperendemic areas such as Rio de Janeiro, Brazil. The disease impact has increased due to changes in epidemiology, necessitating improved prevention strategies, early diagnosis, and tailored treatment plans to reduce its spread and severity.
Conflict of interest: None
Key words: Sporotrichosis; epidemiology; One Health; public health.
Key learning points
- Sporotrichosis is a subcutaneous fungal infection that can be caused by various Sporothrix spp., with S. brasiliensis being the most prevalent in recent outbreaks.
- The disease is primarily transmitted via traumatic inoculation through activities such as gardening or through zoonotic transmission, mainly from cats.
- Although in most cases benign, sporotrichosis is of public health significance due to its social impact, occupational nature, potential for dissemination in vulnerable populations, and recent epidemiological changes.
- Multidisciplinary care is essential, particularly in immunosuppressed patients and when dissemination occurs.
- An integrated approach to human, animal, and environmental health is essential to prevent and control sporotrichosis.
Introduction
Sporotrichosis, caused by Sporothrix spp., is an endemic subcutaneous fungal infection, classified as an implantation mycosis. The infection is typically caused by traumatic inoculation of the fungus into the skin through activities such as gardening or agriculture, or via zoonotic transmission, particularly from cats.1 The most clinically significant and frequently implicated species in human infections are S. schenkii, S. brasiliensis, S. globosa, S. mexicana and S. luriei.2 Although the infection is largely non-fatal, remaining localized to the skin, sporotrichosis is of public health significance due to its social impact, occupational nature, potential for dissemination in vulnerable populations, and the epidemiological changes that have been observed since the late 1990s. Addressing these challenges requires urgent intervention that integrates human, animal, and environmental health in line with the One Health approach.
Epidemiology
Sporotrichosis is globally distributed, with a higher prevalence in tropical and subtropical regions where environmental and climate conditions favour the spread of the pathogen. The infection occurs endemically in some areas, such as Latin America and China, and outbreaks have been reported in several other countries, including the USA, South Africa, and Australia, most often related to occupational activities such as working in mines, gardening, fish handling, and agriculture. In China, outbreaks of the disease have been reported after floods. 1,3
In recent years, the incidence of sporotrichosis has seen a notable increase, initially in Rio de Janeiro, Brazil. Since 1997, when S. brasiliensis was identified as the primary species implicated in the zoonotic hyperendemic situation in the state, the number of cases has been increasing across Brazil and neighbouring countries.4,5 This upward trend has been observed in hospitalizations and deaths due to sporotrichosis throughout Brazil6 and, as of 2023, more than 14,000 human- and 20,000 feline cases have been officially reported to the authorities in the state of Rio de Janeiro.7
Beyond Brazil, S. brasiliensis has been reported in other countries in the Americas and in Europe, where cases involved patients originating from Brazil. The species has also been found in soil samples in Argentina. However, climate change and shifts in spatial dynamics make it difficult to predict with certainty which countries, and at what point in time, conditions conducive to the emergence of new outbreaks will arise.7
Clinical presentation
Cutaneous sporotrichosis is the most common clinical form. Most patients (75–80%) present with the lymphocutaneous form (Figs 1 and 2), characterized by an initial lesion at the inoculation site, usually ulcerated, and similar lesions that follow an ascending lymphatic distribution. The less common cutaneous clinical form, the fixed cutaneous form (Fig. 3), is characterized by a single ulcerated lesion, sometimes vegetative, at the site of inoculation, typically associated with small satellite lesions.1

Due to the increasing number of cases caused by the highly virulent S. brasiliensis, atypical clinical forms and hypersensitivity reactions have been reported with greater frequency, particularly in Rio de Janeiro. Erythema nodosum, Sweet’s syndrome, erythema multiforme, and reactive arthritis have been observed in association with both cutaneous and extracutaneous disease presentations.5
Ulcerated lesions, as well as sporotrichoid presentation, may occur in a range of differential diagnoses, including cutaneous leishmaniasis, mycobacterial infections, other mycoses, and even neoplasms. Clinical history and epidemiological context should be considered, and appropriate laboratory tests performed.1

In addition to cutaneous forms, sporotrichosis may affect the skeletal system (via contiguous spread or dissemination) as well as the lungs, eyes, and central nervous system. Systemic involvement is more commonly observed in immunosuppressed patients and is frequently reported in people living with human immunodeficiency virus (HIV). Systemic involvement should be investigated in immunosuppressed or symptomatic patients, requiring a comprehensive multidisciplinary approach that includes radiography of the chest, long bones, or those contiguous with the lesion, as well as ophthalmological, otorhinolaryngological, and neurological examinations. 5,8
The most used and reliable test for diagnosis is the culture of tissue or lesion exudate. Direct mycological examination is negative in most cases. While serology, molecular tests, and lateral flow assays are promising and available in research services, they are not widely available.7

Treatment
Itraconazole is the drug of choice for the treatment of sporotrichosis (Table 1). The dosage may range from 100 to 400 mg depending on clinical manifestations, comorbidities, and treatment response. In general, treatment lasts for a minimum of three months. However, longer treatment durations have been observed in infections caused by S. brasiliensis. Itraconazole is a strong inhibitor of CYP3A4 and therefore has numerous potential drug interactions. A comprehensive patient history should be obtained, and temporary discontinuation of other drugs may be considered.1,9
Potassium iodide, although an older and no longer widely used drug, has an immunomodulatory effect in sporotrichosis and demonstrates good efficacy. It is particularly used in children and in the treatment of hypersensitivity forms during hyperendemic situations. The recommended dosage is 2.8 to 3.5 g per day, divided into two to three doses. Gastrointestinal intolerance is the main reason for discontinuation, and thyroid function should be monitored during treatment.9
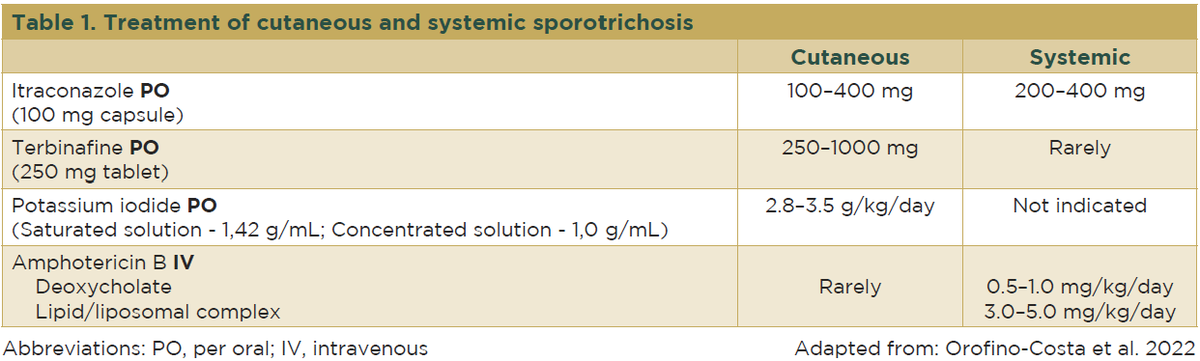
Increasing rates of non-wild type S. brasiliensis – which demonstrate reduced susceptibility to itraconazole – have been observed, which is concerning given the limited range of treatments available. In patients with contraindications to itraconazole, or in cases of therapeutic failure, terbinafine may be used at a dose of 250 to 1000 mg per day for a similar duration.9,10
Cryosurgery, thermotherapy, electrosurgery, or excision may be used as adjuvant therapies in cases of poor therapeutic response or when other medications are contraindicated, such as during pregnancy.5,9
In more severe cases involving dissemination, particularly in immunosuppressed patients, amphotericin B, ideally in liposomal formulations, should be used at a dose of 3 to 5 mg/kg/day. Treatment regimens suggested in the literature vary according to clinical situation and range from daily administration for 2 to 6 weeks to intermittent dosing a few times per week. Until symptoms improve, the patient should continue treatment with itraconazole.9,8
Cases of hypersensitivity secondary to sporotrichosis generally respond well to antifungal treatment; however, non-steroidal anti-inflammatory drugs (NSAIDs) or corticosteroids may be added in more symptomatic cases. Due to its immunomodulatory activity, potassium iodide may be a suitable treatment option in such cases.5,9
Prevention and control
Preventive measures include wearing protective clothing and gloves while handling soil, plants, or clinically affected cats, and practicing recommended wound care. Public health initiatives should focus on the One Health approach, educating the community about the risks associated with zoonotic transmission and the importance of seeking prompt medical attention for suspicious skin lesions. It has been demonstrated that S. brasiliensis can survive in the environment on materials such as stainless steel and wood for up to 25 days – although further investigation is needed, this finding suggests the potential for fomite transmission. Strategies to reduce transmission include the diagnosis and treatment of infected cats, public awareness campaigns promoting responsible pet ownership, the use of personal protective equipment when handling symptomatic animals, and the proper disposal of deceased felines to reduce environmental contamination. Sporotrichosis became a notifiable disease in Brazil in March 2025.
Conclusion
Sporotrichosis remains a significant public health issue, particularly in endemic regions. Continued surveillance, research, and public health efforts are essential in controlling the spread of this infection and reducing its impact on affected populations. Additionally, an integrated approach to human, animal, and environmental health is essential. A well-implemented One Health approach can contribute to the prevention and control of the disease, both in areas where it is already well established and in regions that may subsequently become affected.
Acknowledgements
We would like to express our thanks to the residents Maria Lúcia Paysano and Roberta Nicol D’cunha for their assistance with the selection of photographs.
References
- Barros MB, Almeida-Paes R, Schubach AO. Sporothrix schenckii and sporotrichosis. Clin Microbiol Rev 2011; 24:633–54.
- Zhou X, Rodrigues AM, Feng P, Hoog GS. Global ITS diversity in the Sporothrix schenckii complex. Fungal Divers 2014; 66:153–65.
- Chakrabarti A, Bonifaz A, Gutierrez-Galhardo MC et al.Global epidemiology of sporotrichosis. Med Mycol 2015; 53:3–14.
- Barros MB, Schubach TM, Gutierrez-Galhardo MC, et al. Sporotrichosis: an emergent zoonosis in Rio de Janeiro. Mem Inst Oswaldo Cruz 2001; 96:777–9.
- Schechtman RC, Falcão EMM, Carard M et al. Sporotrichosis: hyperendemic by zoonotic transmission, with atypical presentations, hypersensitivity reactions and greater severity. An Bras Dermatol 2022; 97:1–13.
- Falcão EMM, de Lima Filho JB, Campos DP et al. Hospitalizações e óbitos relacionados à esporotricose no Brasil (1992–2015). Cad Saúde Pública 2019; 35:e00109218.
- Almeida-Paes R, do Valle ACF, Freitas DFS et al. The present and future research agenda of sporotrichosis on the silver anniversary of zoonotic sporotrichosis in Rio de Janeiro, Brazil. Mem Inst Oswaldo Cruz 2024; 119:e230208.